What is Bone Augmentation?
Alveolar bone defects may result from congenital malformations, traumatic injuries, periodontal disease, surgical trauma, chronic periapical lesions and benign or malignant tumors. The causes of resorption of the alveolar bone after tooth loss, are related to its atrophy due to loss of function, reduced blood supply, local inflammation or inadequate pressure from the prosthetic device. After the loss of teeth, the resorption process of the alveolar bone begins with the fastest rhythm in the first few years and with predictable flow – the labial part of the alveolar process is the place of the fastest resorption, with the largest reduction in the transverse and vertical direction. Bone resorption is thought to be 40-60% during the first three years of teeth loss, and then decreased by 0,25-0,5% of the total lost.
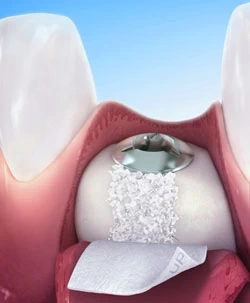
The best strategy in the prevention of alveolar resorption is certainly prevention of its occurrence – tooth loss. If tooth extraction is necessary, preservation should be made – preventive fulfillment of the alveolus with a graft material, immediately after extraction. For successful alveolar regeneration, it is necessary to perform certain subsequent steps:
- Creation of adequate space;
- Protection of the blood coagulum;
- Perforation of the cortico-trabecular part for increased attraction of vascular, cellular and molecular elements required for regenerative process;
- The use of a barrier membrane for the prevention of tissue invasion that can compromise the regeneration.
This criterion is successfully applied to create bone in extraction wounds in deficient alveolar ridges, with a significant increase in the alveolar ridge, especially when it comes to defects in buccal lamina, I which case augmentation is necessary.
Some of the methods of preserving and reconstructing the alveolar ridge today are overcome and can only be a temporary solution. Instead of them, the immediate placement of dental implants in an existing alveolar bone, or delayed implantation in the grafted alveolar bone, is a usual choice in the reconstruction of the dentoalveolar skeleton. The importance of bone preservation, when it comes to the alveolar bone, is imposed as priority, and therefore reconstructive techniques and materials of human and non-human origin are used and developed on a daily basis.
Methods of augmentation of an existing alveolar bone
There are numerous techniques that allow maximizing the available alveolar bone, without using bone grafts. Osteocondensation – one of the techniques that can alter the morphology of the alveolar bone with condensation of the bone in various directions, using appropriate osteotomies.
“Crestal split” technique
– another method that achieves the expansion of an existing alveolar ridge, by making a greenstick fracture on the alveolar base. The greatest benefit of this technique is the possibility to expand a thin alveolar ridge to a width that is sufficient to accommodate implants, without using bone grafting.
Guided bone regeneration (GBR)
– used for small augmentation procedures. The technique is in fact prevention of soft tissue growing into the bone defects, using bone substituent materials and resorptive (collagen) and non-resorptive (metal or titanium) membranes.
Distraction osteogenesis
– used on long bones in children, to extend the bone without bone graft. In the oral and maxillofacial region, it is used as an augmentative technique with making a bone fracture which results with an empty space that initially closes with callus and later matures into bone tissue. The alveolar ridge distraction is initiated from the second to the seventh day of primary osteotomy and ranges daily from 0,25mm to 0,5mm, it is performed continuously for 30 days (with a final result of + 4-7mm new bone tissue).


